The intersection between existing medications and psychedelic therapy represents a significant blind spot that may be silently undermining therapeutic potential for millions of people.
Recent major real-world survey: the majority of users don’t experience the transformative benefits that capture headlines.1
The growing interest in psilocybin therapy has generated significant hope for those struggling with treatment-resistant depression, anxiety, and other mental health conditions. However, a closer examination of recent and robust real-world evidence reveals a concerning reality: the majority of users didn’t experience the transformative benefits that capture headlines.1 Furthermore, a concerning portion of those experiencing a difficult journey go on to suffer through years of persistent difficulties.2 These findings raise a lot of questions and might be explained by a lot of variables—for example, using psychedelics alone and without support is one major and consistent link to negative outcomes. But there is at least one critical gap that remains unassessed in any current research: the impact of everyone’s pharmaceuticals on the outcomes of a psychedelic journey. In other words: What if neutral, negative and unexpected outcomes were the result of unrecognized drug interactions?
Beyond Psychotropics: The Broader Drug Interaction Landscape
Most discussions about psilocybin drug interactions focus narrowly on psychiatric medications—SSRIs, antipsychotics, and mood stabilizers. But this represents only the tip of the iceberg. Through my clinical analysis and development of a comprehensive interaction database, I’ve identified concerning interactions with medications that most would never suspect could impact their psychedelic experience.3,4
The reality is that drug interactions extend far beyond the psychiatric realm. Common medications for weight loss and diabetes, blood pressure management, immune suppression, and even some muscle relaxants can alter psilocybin’s effects or create unexpected safety risks.3,4 These “non-psychotropic” interactions are largely absent from current research and clinical protocols, yet they may be contributing substantially to the unexpected and perhaps disappointing real-world outcomes we’re seeing.
Consider the scope of potential interactions: Americans take medications for cardiovascular health, metabolic disorders, autoimmune conditions, pain management, sleep disorders, and countless other conditions. Each medication represents a potential interaction that could explain why someone’s carefully planned psychedelic journey turns neutral, difficult or even dangerous, or leaves lasting negative effects. When we limit our focus to just psychiatric medications, we’re missing the forest for the trees.
This broader interaction landscape becomes even more critical when we consider the demographics of people seeking psilocybin therapy—often individuals with complex medical histories who have tried conventional treatments without success. These are precisely the people most likely to be taking multiple medications that could interfere with their healing journey.
With over 60% of American adults taking at least one prescription medication and more than a quarter taking four or more5, the intersection between existing medications and psychedelic therapy represents a significant blind spot that may be silently undermining therapeutic potential for millions of people.
The Reality Check: Most Don’t Experience Clear Benefits
The 2024 National Survey Investigating Hallucinogen and Trends (NSIHT) represents the most comprehensive and robust examination of adult psychedelic use in the United States. Notably, this study recruited from a neutral population to provide an unbiased snapshot of real-world psilocybin experiences that avoids psychedelic enthusiasts and critics.1
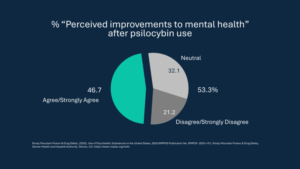
The results are a bit sobering: less than half, or 46.7% of psilocybin users agreed or strongly agreed that the experience improved their mental health.1 This means that 53.3%—the majority—did not experience clear mental health benefits. Even more concerning, 21.2% actively disagreed that psilocybin improved their mental health, while 32.1% remained neutral.1
These findings stand in stark contrast to the 80-90% response rates commonly reported in controlled clinical trials6 and the “generally favourable” outcomes reported in Global Drug Surveys.7 However, even the latter reported negative effects in 22.5% of respondents.7
Furthermore, the NSIHT data revealed that 28.8% of psilocybin users consumed alcohol during their experience, and 37.9% combined it with cannabis.1 These substances are known to diminish, or add risk to, the psilocybin journey experience and extended outcomes.4 These statistics highlight a critical disconnect: while clinical trials carefully control for drug interactions and minimize risk through screening or washout periods, real-world use occurs within a complex pharmacologic landscape with little safety oversight. This gap suggests that uncontrolled and unmanaged medication and substance interactions in real-world settings may significantly influence outcomes.
When Good Intentions Go Wrong: Extended Difficulties
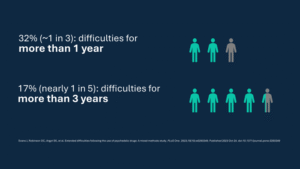
The concerning outcomes don’t end with neutral experiences. A comprehensive, real-world mixed methods study examining 608 participants who reported persistent problems lasting beyond 24 hours after difficult psychedelic experiences found that about 1 in 3 (32%) experienced difficulties lasting more than one year, and almost 1 in 5 (17%) faced problems persisting for over three years.2
While many factors may contribute to these statistics, none of the current research is examining co-existing medications and supplements as potential contributing factors. This represents a significant gap in our understanding of what makes psychedelic experiences go wrong.3
How Medications Can Sabotage Therapeutic Effects
Serotonin System Interference: Many antidepressants, particularly serotonergic ones like selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), can significantly impact psilocybin’s effects. A landmark 2023 study found that among 611 reports of taking psilocybin with an antidepressant, there was a 47% probability of experiencing weaker than expected drug effects with SSRIs and a 55% probability with SNRIs, compared to only 29% with the non-serotonergic antidepressant bupropion.8 Additionally, this dampening effect may persist up to 3 months following antidepressant discontinuation.8 This finding aligns with research analyzing 443 Reddit posts, which found that 54% described reduced intensity of the psilocybin experience with SSRI use, though importantly, 39% reported no change in intensity.9 Regardless of the presence or intensity of subjective effects, a 2025 scoping review of 18 studies found that the concomitant use of antidepressants and classic psychedelics appears generally safe and tolerable, with no increased risk of serotonin syndrome, particularly for psilocybin.10 Thus, while the risk of toxicity appears low when combining a serotonergic agent with psilocybin, the subjective effects and potential therapeutic outcomes are not always certain.
Delayed Absorption Issues: Medications like GLP-1 agonists (Ozempic®, Wegovy®) slow gastric motility as a primary mechanism11, potentially delaying psilocybin’s onset by several hours. This risk appears more likely when the GLP-1 agonist is first started, or the dose is recently increased, or when gastrointestinal symptoms such as nausea, constipation or bloating are present. I first encountered this interaction in early 2025 following a request from a psychedelic provider for a clinical case analysis and have since received similar reports from other practitioners in the field. This delayed onset can lead users to believe the psilocybin isn’t taking effect, only for the experience to begin hours later in a potentially unsafe context, such as while driving. Alternatively, users may take additional doses, assuming the first was ineffective, resulting in unexpectedly intense experiences hours later. This highlights the need for careful review and safety planning to minimize or avoid this interaction using an approach that is safe and effective for the individual. Longer facilitation is often planned, but with the right strategies and medication preparation, that approach may be unnecessary.
Cardiovascular Complications: Consider the case of midodrine (ProAmatine®), a medication for orthostatic hypotension that carries an FDA black box warning for dangerous increases in blood pressure when lying down, with potential for systolic pressures exceeding 200 mmHg12. When combined with a large dose of psilocybin, which can increase blood pressure by 15-20 points13 and which typically requires participants to lay down throughout the experience, this interaction represents a contraindication due to potential hypertensive emergency and significant cardiovascular risk. However, this apparent contraindication can be expertly managed and the risk avoided through careful review, deep pharmacologic understanding, and safety plans designed by a pharmacist.
Acid Reintroduction Problems: A critical misunderstanding involves the advice for people taking antacids or proton pump inhibitors (PPIs) like omeprazole to consume psilocybin with acidic preparations like lemon juice or “tek.” The flawed reasoning suggests that since these medications reduce stomach acid, we must artificially reintroduce acid to aid mushroom digestion and facilitate psilocybin conversion to psilocin. This approach is both scientifically unfounded and potentially harmful to people with acid-sensitive conditions like acid reflux, acid erosion, or ulcers. The science shows that mechanical breakdown through chewing and grinding is likely to play a far more significant role than stomach acid or other acidic medium in the breakdown of mushrooms’ chitinous cell walls and other cellular components to facilitate release of psilocybin. Additionally, the conversion of psilocybin to psilocin primarily occurs through dephosphorylation via alkaline phosphatase enzymes in neutral-alkaline organs and tissues, not through acid hydrolysis.14,15 Actually, the phosphate ester bond that is necessarily cleaved to form psilocin from psilocybin is relatively stable in acidic conditions.16,17 Thus, acid reintroduction is likely unnecessary for either digestion or molecular conversion. Notably, an appreciable number of real-world reports (Reddit, for example) documents full psilocybin experiences in people taking PPIs without any acidic preparation.
The Pharmacist Advantage: Evidence for Professional Consultation
The weight of all this evidence suggests that determining the most appropriate strategy for management of medications and other substances around a journey requires nuanced considerations and personalized guidance and planning to avoid negative, neutral or unexpected outcomes. However, the value of professional medication review extends far beyond psilocybin interactions. A landmark study found that pharmacist participation in patient rounds reduced preventable adverse drug events by 66%.18 Nearly 99% of pharmacist recommendations were accepted by physicians, demonstrating both accuracy and practical value.18
This effectiveness translates across healthcare settings, with meta-analysis evidence showing pharmacist interventions reduce medication error rates by more than 60% compared to usual care, with some studies documenting risk reductions of up to 20-fold.19
Taking Action: A Practical Framework for Safety
Complete but Confidential Pharmacologic Disclosure: Create a comprehensive list including all prescription medications, over-the-counter vitamins, supplements, herbal products and other substance utilization—including alcohol, nicotine, caffeine, cannabis and others.
Professional Review: Consult with a pharmacist familiar with psychedelic interactions.
Strategic Timing: Some medications or substances may need modifications before psilocybin use, and many don’t require tapering. This requires personalized review, guidance and planning for best outcomes rather than blanket avoidance or discontinuation recommendations.
The Path Forward: Evidence-Based Safety
The convergence of real-world outcome data and pharmacologic evidence suggests that unaddressed pharmacologic interactions may be silently shaping many of the disappointing or prolonged difficulties seen in practice.
The appropriate response is not to discourage exploration of psilocybin’s therapeutic potential, but to strengthen harm reduction and safety measures surrounding its use—particularly as more individuals pursue it in clinical, research, unregulated and emerging regulated contexts. Comprehensive pharmacologic review and evidence-based interaction screening should be viewed not as gatekeeping measures, but as essential tools to reduce risk and preserve the possibility of therapeutic benefit.
For those considering psilocybin therapy, consulting with a qualified healthcare professional about potential pharmacologic interactions represents a key harm reduction step. Identifying and managing these risks may mean the difference between a well-tolerated, potentially beneficial experience and one that leads to discouragement or enduring difficulty.
The evidence is clear that in our complex polypharmacy landscape, beyond preventing negative experiences and outcomes, checking and managing pharmacologic interactions is a matter of reducing harm and supporting informed, safer pathways toward healing and self-understanding.
References:
- Rocky Mountain Poison & Drug Safety. Use of Psychedelic Substances in the United States, 2024 NSIHT Report. RMPDS Publication No. RMPDS-2025-I-01. Rocky Mountain Poison & Drug Safety, Denver Health and Hospital Authority. Denver, CO. 2025. Available at: https://www.rmpds.org/nsiht
- Evans J, Robinson OC, Argyri EK, et al. Extended difficulties following the use of psychedelic drugs: A mixed methods study. PLoS One. 2023;18(10):e0293349. Available at: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0293349
- Speer K. Beyond Psychotropics: Relevant Psilocybin Interactions You Don’t Want to Miss. Collaborence Conference Presentation, Boulder, CO. October 4-5, 2025.
- The Psilocybin Mushroom Interaction Checker. Available at: https://www.psychedelicinteraction.com
- Kaiser Family Foundation. Public Opinion on Prescription Drugs and Their Prices. Published October 4, 2024. Accessed October 1, 2025. https://www.kff.org/health-costs/poll-finding/public-opinion-on-prescription-drugs-and-their-prices
- Goodwin GM, Aaronson ST, Alvarez O, et al. Single-dose psilocybin for a treatment-resistant episode of major depression. N Engl J Med. 2022;387(18):1637-1648. Available at: https://www.nejm.org/doi/full/10.1056/NEJMoa2206443
- Molnar A, Simon N, Tomori DV, et al. Investigation of self-treatment with lysergic acid diethylamide and psilocybin mushrooms: Findings from the Global Drug Survey 2020. J Psychopharmacol. 2023;37(3):296-308. Available at: https://journals.sagepub.com/doi/10.1177/02698811231158245
- Gukasyan N, Griffiths RR, Yaden DB, Antoine DG 2nd, Nayak SM. Attenuation of psilocybin mushroom effects during and after SSRI/SNRI antidepressant use. J Psychopharmacol. 2023;37(7):707-716. doi:10.1177/02698811231179910
- Gukasyan N, Nayak SM, Griffiths RR, et al. Content analysis of Reddit posts about coadministration of selective serotonin reuptake inhibitors and psilocybin mushrooms. Psychopharmacology. 2024;241(8):1617-1630. Available at: https://link.springer.com/article/10.1007/s00213-024-06570-7
- Tap SC, Thomas K, Páleníček T, et al. Concomitant use of antidepressants and classic psychedelics: A scoping review. J Psychopharmacol. 2025 Sep 12:2698811251368360. Available at: https://journals.sagepub.com/doi/10.1177/02698811251368360
- Marathe CS, Rayner CK, Jones KL, Horowitz M. Effects of GLP-1 and incretin-based therapies on gastrointestinal motor function. Exp Diabetes Res. 2011;2011:279530. doi:10.1155/2011/279530
- ProAmatine® (midodrine hydrochloride) [package insert]. Lexington, MA: Shire US Inc; Revised January 2017.
- Holze F, Ley L, Müller F, et al. Direct comparison of the acute effects of lysergic acid diethylamide and psilocybin in a double-blind placebo-controlled study in healthy subjects. Neuropsychopharmacology. 2022;47(6):1180-1187. Available at: https://www.nature.com/articles/s41386-022-01297-2
- HORITA A, WEBER LJ. The enzymic dephosphorylation and oxidation of psilocybin and psilocin by mammalian tissue homogenates. Biochem Pharmacol. 1961;7:47-54. doi:10.1016/0006-2952(61)90124-1
- Eklund J, Bremberg U, Larsson J, et al. Synthesis and In Vitro Profiling of Psilocin Derivatives: Improved Stability and Synthetic Properties. J Med Chem. 2025;68(7):7153-7165. doi:10.1021/acs.jmedchem.4c02612
- Lassila JK, Zalatan JG, Herschlag D. Biological phosphoryl-transfer reactions: understanding mechanism and catalysis. Annu Rev Biochem. 2011;80:669-702. doi:10.1146/annurev-biochem-060409-092741
- Wolfenden R, Snider MJ. The depth of chemical time and the power of enzymes as catalysts. Acc Chem Res. 2001;34(12):938-945. doi:10.1021/ar000058i
- Leape LL, Cullen DJ, Clapp MD, et al. Pharmacist participation on physician rounds and adverse drug events in the intensive care unit. JAMA. 1999;282(3):267-270. Available at: https://jamanetwork.com/journals/jama/fullarticle/190687
- Gillam SW, Choi I, King KH, Nelson KM, Patel KI. Impact of pharmacist intervention on the quality of diabetes care and clinical outcomes in patients with complex diabetes. Am J Health Syst Pharm. 2013;70(2):143-152.
If you would like to cite this article, copy the format you need:
AMA (11th ed.)
Speer K. Negative, Neutral or Unexpected Psychedelic Therapy Outcomes Can Be Due to Unrecognized Drug Interactions. PharmD Consult. Published October 12, 2025. Accessed [add current month, day, year, remove brackets]. https://psychedelicinteraction.com/pharmd-consult
APA (7th ed.)
Speer, K. (2025, October 12). Negative, Neutral or Unexpected Psychedelic Therapy Outcomes Can Be Due to Unrecognized Drug Interactions. PharmD Consult. https://psychedelicinteraction.com/pharmd-consult. Accessed [add current month, day, year, remove brackets].
Chicago (17th ed., author-date citation)
Speer, Kristin. 2025. “Negative, Neutral or Unexpected Psychedelic Therapy Outcomes Can Be Due to Unrecognized Drug Interactions.” PharmD Consult, October 12, 2025. Accessed [add current month, day, year, remove brackets]. https://psychedelicinteraction.com/pharmd-consult.
MLA (9th ed.)
Speer, Kristin. Negative, Neutral or Unexpected Psychedelic Therapy Outcomes Can Be Due to Unrecognized Drug Interactions. PharmD Consult, 12 Oct. 2025. Accessed [add current day, month abbreviated, year, remove brackets]. https://psychedelicinteraction.com/pharmd-consult.
Disclaimer
The information provided on this page is for educational purposes only. It should not be used as medical advice. Always follow the advice and direction of your provider(s). Do not attempt to stop or make changes to your medications or care plans on your own, as this can be dangerous. Neither Dr. Speer nor PharmD Consult shall be held responsible or liable for any outcomes related to the use of this information.
